Original in Russian is available at the link: Нижний портал. Часть 1. below is a machine translation edited by a non-native speaker (version dated 03/02/2025).
INFERIOR PORTAL FOR HIP
ARTHROSCOPY: A PILOT STUDY
PART 1. Background and Hypothesis
Arkhipov S.V., Independent Researcher, Joensuu, Finland
CONTENTS
PART 1.
Background and Hypothesis
[1].
Introduction
[2]. Passage through the Inferior Portal
[3].
Main Advantages of the Proposed Technique
[4]. Specific Risks of the Proposed
Technique
[5]. Main Limitations of the Proposed
Technique
[6]. References
(Part 1)
PART 2. Inferior Portal Prototypes
[7]. Open Reduction
[8]. Puncture and Arthrography
[9]. Arthroscopy
and Debridement
[10].
References (Part 2)
[1]. Introduction
Hip arthroscopy is considered a complex and expensive surgical procedure (2015SalasAP). However, it provides a dynamic and accurate assessment of the hip joint, and is recognized as the gold standard for diagnostics (2018JamilM_WittJ). Hip arthroscopy may be one of the last frontiers in sports medicine (2019MaldonadoDR_DombBG).
 |
| Fig. 1. Compartments of the hip joint (schematic); the central compartment is highlighted in red, the peripheral compartment is highlighted in blue (from 1892PoirierPJ, unchanged). |
Traditionally, arthroscopic surgeons of the hip joint distinguish three compartments: the central compartment, the peripheral compartment, and the lateral compartment outside the joint, also known as the peritrochanteric compartment (2008RobertsonWJ_KellyBT). The central compartment of the hip joint contains important structural elements: 1/2 of the femoral head, the fossa, notch, and lunate surface of the acetabulum, synovial folds, fatty tissue, the transverse ligament of the acetabulum, the medial surface of the acetabular labrum, the ligament of the head of the femur, more often referred to in Latin as ligamentum capitis femoris (LCF), or ligamentum teres (Fig. 1). For the arthroscopic approach to the above-mentioned space, the following portals are used: anterior, anterolateral, mid-anterior, distal anterolateral and posterolateral (2016ApratoA_MasseA; 2020TangHC_DienstM) (Fig. 2).
The main condition for penetration into the central compartment is a partial displacement of the femoral head from the acetabulum in the lateral direction. It has been noted that a stretch of 8-10 mm is usually sufficient (2024GursoyS_ChahlaJ). Sometimes the average distraction is 13-15 mm (2011BadylakJS_KeeneJS). For iatrogenic hip subluxation, an operating distractor is used, as well as traction on the operating table with a force of 25 to 200 lb (~11.3-90.7 kg), which corresponds to 112 to 900 N (1995McCarthyJC_BusconiB). However, "traction and the means of distraction remains a potent source of problems for the unwary" (2010SimpsonJ_VillarR). Patient positioning and duration of traction are the primary considerations (2012PapavasiliouAV_BardakosNV).
The literature on complications of this surgical procedure is extensive and illustrates in detail the dangers associated with traction, trauma to neurovascular structures, perineal compression, and external portal placement (2006LoP_ShihCH; 2009MatsudaDK; 2011SaidHG_DienstM; 2012PapavasiliouAV_BardakosNV; 2013ChanK_AyeniOR; 2013KowalczukM_AyeniOR; 2014DippmannC_HölmichP; 2014GuptaA_DombBG; 2016DuplantierNL_HarrisJD; 2016NakanoN_KhandujaV; 2017FrandsenL_LindM; 2017StoneAV_StubbsAJ; 2017DegenRM_LymanS; 2017SeijasR_CugatR; 2018SalasAP_GarciaJM; 2019AyeniOR_KellyBT; 2019BaileyTL_MaakTG; 2025ChiangCC_ChanYS, 2025GüvenŞ_FıratA). Some studies note that negative phenomena caused by traction during hip arthroscopy are found in 74% of patients (2017FrandsenL_LindM). The main problems after treatment of pathology of the central compartment of the hip joint with distraction:
- injuries to the soft tissues of the perineum from the impact of the counter-support (perineal post), causing damage to the external genitalia: edema, hematomas, abrasions, ruptures of the scrotum, vagina, labia minora, skin necrosis;
- neuropraxia: genital, femoral, sciatic, peroneal nerve due to compression or excessive elongation, as well as the lateral cutaneous nerve of the thigh from traction or from the impact of an instrument;
- erectile dysfunction;
- effects on urinary functions;
- obstruction of major arteries at the ankle level;
- pathology of the distal parts of the lower limb in the form of local hypercompression of the skin, prolonged pain and hypoesthesia in the area of the foot, knee and ankle joint;
- damage to the articular cartilage of the femoral head and acetabulum by instruments;
- pinching of the instrument between the femoral head and the acetabulum;
- aseptic necrosis of the femoral head;
- possibly, postoperative subluxation and dislocation of the hip;
- probably, a fracture of the femoral neck without displacement, described as "stress".
The above makes us think about the justification of traction. Normally, the internal opening of the acetabular labrum is smaller than the diameter of the head. The acetabular labrum elastically embraces the head of the femur, holding it in the socket, and seals the central compartment. According to S. Garbe (1998), the width of the acetabular labrum is 10-12 mm. During open operations on the hip joint, we have repeatedly observed a wide acetabular labrum in young subjects, resembling a semi-closed diaphragm of optical instruments. Accordingly, when attempting to examine the central compartment using standard approaches, damage to the acetabular labrum is expected. A sharp spoke or needle can perforate it, and a blunt instrument will at best bend back the elastic edge. Acetabular labrum injuries are an indication for surgical treatment (1999FarjoLA_SampsonTG; 2006BharamS; 2009ParviziJ_PetersC). However, arthroscopy itself in its current form clearly carries a risk of violating the integrity of the structure that we are trying to preserve or restore. Unintentional puncture of the acetabular labrum during arthroscopy is noted in 25% of cases (2011BadylakJS_KeeneJS).
Orthopedic surgeons know how difficult it can be to perform an intraoperative dislocation in the hip joint, for example, when removing the femoral head during hip arthroplasty. or during disarticulation. One of the first vivid descriptions of the difficulties of extracting the femoral head from the acetabulum during hip disarticulation was found in the monograph by К. Грум (1837). The first to study this phenomenon in detail were W. Weber and E. Weber, who showed that the reason was hermetic sealing (1836WeberW_WeberE). There are no open holes in the acetabulum, and the gap between the lunate surface and the femoral head is filled with synovial fluid. In the experiment and during the operation, trying to extract the head from the acetabulum, we thereby spontaneously increase the counteracting hydrostatic pressure in the central compartment. Essentially, the surgeon creates decompression and aims to stretch the synovial fluid. When air gets into the central compartment, the negative hydrostatic pressure inside is replaced by atmospheric pressure and ceases to hinder us. The head begins to yield to traction. Now we must overcome the force of surface tension of the synovial fluid and adhesion, which are associated with intermolecular interaction. Next, it is necessary to "defeat" the force of elastic-elastic pressing of the head by the acetabular labrum and cross the LCF. The multitude of forces simultaneously hindering the surgeon's activity explains the difficulties in the operation of hip disarticulation. If they are overcome, the air rushes noisily into the acetabulum, demonstrating a suction effect (1820PallettaGB; 1836WeberW_WeberE).
To hold the femoral head in a subluxation state, we need to constantly maintain the stretching of the joint capsule and external ligaments, which have a high modulus of elasticity. According to А.С. Обысов (1971), Young's modulus for different ligaments varies from 9.8 N/mm2 to 120.0 N/mm2 (~1.0-12.2 kg/mm). The abducted thigh is in the same direction as the stretched, practically inextensible iliofemoral ligament, which is known to withstand a load of 350 kg (1932ВоробьевВП; 1995МинеевКП). According to В.Н. Воробьев (1972), the iliofemoral ligament begins with a cord reaching 5 cm in width and up to 1-1.5 cm in thickness. Therefore, it is not surprising that rupture of the ligamentous apparatus is observed with a pull of 408-1343 kg, on average 850 kg (1947НиколаевЛП).
It should be remembered that with lateral displacement of the femoral head, the LCF is also stretched. The most optimistic strength of the LCF in humans according to H.H. Chen et al. (1996) is 234 ± 168 N; in the observations of С.О. Малаховой (2001) - 310 N; in the studies of F. Gao et al. (2008) - 216.15 ± 20.00 N; according to M.J. Philippon et al. (2014) - 204 ± 128 N; in the experiments of Е.П. Подрушняк (1972), in young people it is 56.4±14.0 kg (or 552.72±137.2 N). Thus, traction over 690 N is highly likely to partially disrupt the integrity of the mentioned anatomical structure. Weakening of the LCF, in our opinion, is one of the prerequisites for hip dislocation after hip arthroscopy (2009MatsudaDK; 2016DuplantierNL_HarrisJD).
The force that the traction device of the operating table has to apply is very high. According to Newton's third law, the body presses on the counter-support with a similar force. As we remember, this is 11.3-90.7 kg or 112-900 N (1995McCarthyJC_BusconiB). The soft tissue organs of the perineum are not adapted to such impressive pressure. When stretched with this force for less than one hour, the nerves also suffer (2019BaileyTL_MaakTG). It is not surprising that this results in ruptures and necrosis of the skin. In addition, the nerves are compressed and excessively overstretched, in the first case - the pudendal nerve and cutaneous nerves of the ankle joint, and in the second - the femoral, sciatic and peroneal nerves. The authors who studied traction injury of the sciatic nerve, detected in 65% of patients (!), recommended trying to minimize the load and time of traction during hip arthroscopy (2012TelleriaJJ_GlickJM). It is generally accepted that distraction should not exceed two hours (2024GursoyS_ChahlaJ).
 |
| Fig. 4. Probe inserted into the opening under the transverse ligament of the acetabulum (from 1794LoderJC, unchanged). |
The above prompted the author to search for ways to minimize complications from traction during hip arthroscopy. By 2004, we had formed an idea of the acetabular canal (2004Архипов-БалтийскийСВ). It is formed by the head of the femur, as well as the fossa and notch of the acetabulum (for more details, see Acetabular Canal. Part 1). This is an open, blindly ending slit-like space. It can be accessed through an opening under the transverse ligament of the acetabulum. After 2004, the idea of examining the central compartment of the hip joint through the acetabular notch using an arthroscope arose. The idea was postponed, but thoughts about this approach did not cease (Fig. 3).
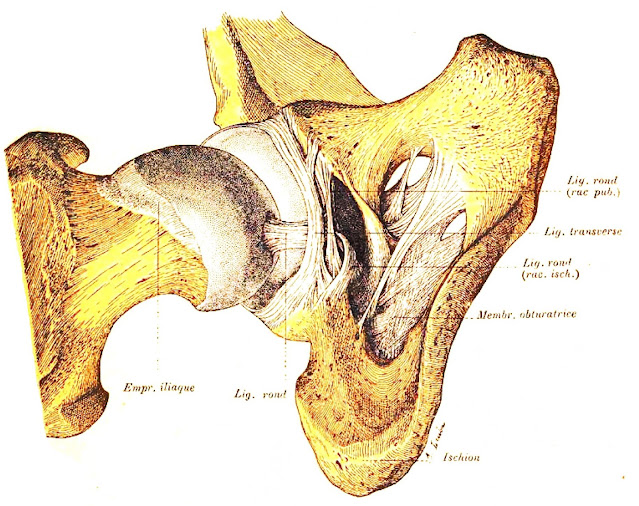 |
| Fig. 5. "Entrance" of the LCF into the hip joint through the acetabular canal; top – from 1890DebierreC (unchanged); bottom – from 1892PoirierPJ (unchanged). |
Literary research has shown that our ideas were not original. T. Schwencke inserted a tube into the canal under the transverse ligament and pumped air into it, as reported in the monograph Haematologia (1743). J.C. Loder was the first to depict a probe in the acetabular canal in his monograph Tabulae anatomicae (1794) (Fig. 4). G.B. Palletta described the introduction of a needle into the "oval opening" under the transverse ligament in Exercitationes pathologicae (1820). The synovial membrane covering the LCF and fatty tissue was outlined as a tube coming out through the acetabular notch by C.T. Aeby (1868). The LCF entering the acetabular canal was shown in the figure by C. Debierre (1890) and also by P.J. Poirier (1892) (Fig. 5). The direction of penetration into the acetabular fossa through the opening under the transverse ligament was indicated in monograph by L. Testut (1904) (Fig. 6). J.E.S. Fraser (1920), explaining the formation of the LCF, wrote: «Thus, a synovial funnel is formed, wider below where it includes the attachment of the fibres [LCF], and narrowed at its femoral end, where it is fastened to the fovea.».
 |
| Fig. 6. Arrow indicates the entrance to the right acetabular canal under the transverse ligament of the acetabulum; legend: 1 — pubic bone, 1’ — pubic spine; 2 — ischium; 3 — ilium; 4 — acetabulum, 4’ — acetabular margin; 5 — capsule resected at the level of the labrum; 6 — obturator membrane, 6’ — accessory bundle; 7 — subpubic ligament; 8 — subpubic (obturator) canal; 9 — opening occupied by fat lobules; 10 — ischiopubic opening (from 1904TestutL, unchanged). |
[2]. Passage through the Inferior Portal
From our perspective, for examining the central compartment of the hip joint, it is advisable to introduce the arthroscope's optical system through the acetabular canal using the inferior portal (approach).
 |
Fig. 7. Schematic representation of the patient on the operating table with an approximate indication of the point of the inferior portal for hip arthroscopy.
 |
Fig. 8. Approximate position of the patient on the operating table with an image of the flexion of the operated leg as represented by artificial intelligence (the figure was created by ChatGPT-4o at our request, there are several discrepancies with reality that are not related to the essence of the figure).
We recommend positioning the patient on the operating table in a supine position. Both legs are spread by 40-50º, and the operated thigh is flexed at the hip joint by 10-15º, maintaining neutral rotation (Fig. 7, 8). To insert a guide pin, needle or trocar, an incision in the skin should be made on the medial surface of the thigh across the long axis of the segment 40-50 mm below the inguinal fold. The designated point is above the site of perforation of the fascia by the cutaneous branch of the obturator nerve (r. cutaneus n. obturatorius) and lateral to the pudendal nerve (n. pudendus). Here the skin is mainly innervated by the branches of the posterior cutaneous nerve of the thigh (n. cutaneus femoris posterior). The long adductor muscle (m. adductor longus), the gracilis muscle (m. gracilis) and the obturator vascular-nerve bundle will be located above the skin incision. In the proposed area of approach to the hip joint, there are no large arterial and venous vessels, as well as lymphatic collectors, but inguinal lymph nodes (nn. limphatici inguinales superficiales et profundi) may be present. Below and laterally runs the posterior accessory saphenous vein (v. saphena accessoria posterior). Deeper lie the muscular branches of the obturator artery and vein (a. et v. obturatoriae), as well as the branches of the medial circumflex femoral artery and veins (a. et vv. circumflexa femoris medialis) (Fig. 9). We have compared the anatomy of nerves and vessels with the fundamental works of: H. Gray (1908), В.В. Кованов, А.А. Травин (1963), Р.Д. Синельников, Я.Р. Синельников (1996), F. Netter (2011).
 |
| Fig. 9. Frontal incision of the hip joint passing through the fovea capitis femoris (frozen preparation, right side, posterior segment of the incision), there is no abduction in the hip joint, we have schematically added an arthroscope; legend: 1 — head of the femur; 2 — acetabulum, 2’ — its bottom; 3 — acetabular rim, 3’ —ligamentum transversum; 4 — LCF; 5 — joint capsule; 6 — iliopsoas muscle with serous bursa; 7 — gluteal aponeurosis; 7' — serous bursa of gluteus maximus; 8 — gluteus medius; 9 — gluteus minimus; 10 — piriformis tendon; 11 — tendon of the internal obturator muscle; 12 — tendon of the external obturator muscle (12’); 13 —vastus lateralis; 14 —vastus medialis; 15 — pectineus muscle; a — external iliac vessels; b — deep femoral artery and vein; c — medial circumflex femoral vessels; g — obturator vessels and nerve (from 1904TestutL, with our additions). |
 |
| Fig. 10. Human pelvis, front view; we have added the position of the arthroscope (exhibit of the Zoological Museum of Moscow State University, Moscow, photograph by the author). |
Under the dermis there is subcutaneous fat and superficial fascia of the thigh. The guide pin should be oriented cranially, forward and inward by 10º (Fig. 10, 11). Moving along the indicated trajectory, we will encounter the large adductor muscle (m. adductor magnus), and then the external obturator muscle (m. obturatorius externus). Our goal is the external opening of the acetabular canal (Fig. 12). T. Schwencke (1743) called it the "oval opening" (foramen ovale). In the front view, the transverse ligament and the outer edges of the acetabular notch actually form a rounded, elongated opening (Fig. 13). The opening also has an oval shape in CT. However, in this case, the outer edge is formed by the lower surface of the femoral head (Fig. 14).
 |
| Fig. 12. External opening of the acetabular canal (indicated by the arrow); 3D reconstruction of computed X-ray tomography; front view (personal observation). |
 |
| Fig. 14. External opening of the acetabular canal (arrow); 3D reconstruction of a computed tomography, inferior view (personal observation). |
For experimental entry into the acetabular canal, we modified Synbone company models of the pelvis and femur, made to a 1:1 scale from foam polymer. In particular, congruent articular surfaces of the femoral head and acetabulum were added, the transverse ligament and acetabular labrum were formed (Fig. 15). This is how the external opening of the acetabular canal was recreated (Fig. 16).
We simulated the insertion of the sheath and arthroscope into the acetabular canal on the model (Fig. 17). The outdated endoscope used allowed the cutting instrument to be inserted into the central compartment (Fig. 18, 19). Thus, single-portal arthroscopy of the hip joint using the lower approach was simulated in the experiments. A similar technique was proposed for the knee joint (2013CooperDE_FoutsB).
 |
| Fig. 17. Reproduction of arthroscope insertion into the central compartment of the hip joint on a modified Synbone pelvis model (experiment and photograph by the author). |
 |
| Fig. 18. Reproduction of the insertion of an arthroscope and scissors into the acetabular canal of the model on a modified Synbone pelvis and femur model (experiment and photograph by the author). |
 |
| Fig. 19. Reproduction of the insertion of an arthroscope and scissors into the central compartment of the hip joint on a modified Synbone pelvis model (experiment and photograph by the author). |
When introducing the guide pin to the opening of the acetabular canal, caution and control by means of multiposition fluoroscopy are assumed. Between the inner surface of the external obturator muscle (m. obturatorius externus) and the lower anterior edge of the acetabulum there is fatty tissue in which arteries, veins and lymphatic vessels pass. Of particular importance are: the acetabulum branch (r. acetabularis) – a continuation of the medial circumflex femoral artery (a. circumflexa femoris medialis), as well as the terminal element of the posterior branch of the obturator artery (r. posterior a. obturatoria), also called the acetabulum branch (r. acetabularis) (1963КовановВВ_ТравинАА; 1996СинельниковРД_СинельниковЯР). A branch of a. acetabuli r. posterior a. obturatoria is a. lig. capitis femoris (a. lig. teres), which ends as the medial epiphyseal artery (1965ChapchalG; 1984SteinbergME). The posterior branch of the obturator nerve (r. posterior n. obturatorius) approaches the acetabulum notch from the front, namely from the side of the external opening of the obturator canal (Fig. 20) (1857RudingerN; 1935ГеселевичАМ; 1977ПерлинБЗ_БибиковаЛА; 1981ГолубДМ_БронивицкаяГМ). In order to exclude injury to blood vessels and nerves, it is justified to use a guide pin without cutting edges.
 |
| Fig. 20. Branches of the medial circumflex femoral artery, the obturator artery, and the obturator nerve (from 1908GrayH, unchanged). |
In the area of the posterior wall of the peripheral part of the acetabular canal, a powerful sciatic bundle LCF begins (Fig. 5). In this regard, one should try to insert the pin (needle, trocar) into the anterior part of the external opening of the acetabular canal (Fig. 21). Before the guide device enters the acetabular canal, it is reasonable to perform internal rotation of the femur in the hip joint. The above technique will stretch the synovial membrane and the anterior synovial fold to facilitate their puncturing. The main thing is that the LCF will move to the posterior part of the acetabular fossa. This will reduce the likelihood of puncture damage to the LCF.
 |
| Fig. 21. Shows arthroscope insertion anterior to the LCF; acetabular floor removed (from 1904FickR, with our addition and image rotation). |
The cross-section of the acetabular canal is variable. In the area of the external opening, it is wider than in the middle of the peripheral section. Bypassing this area, the acetabular canal begins to widen. In the final part of the central section, its width and depth decrease (Fig. 22).
The acetabular canal ends blindly with the walls of the acetabular fossa and the edges of the semilunar surface. Therefore, the advancement of the pin (trocar, needle) here is also important to constantly monitor using fluoroscopy. Having made sure that the guide device has been inserted into the central section of the acetabular canal, an arthroscopic sheath with a diameter of 4 mm is inserted according to the standard procedure. Next, the pin (wire) is removed and replaced with an endoscope. After replacing the pin with a sheath with an optical system, we should see the arthroscope directly in the acetabular canal on the fluorogram (X-ray) (Fig. 23).
The depth of the acetabulum fossa, i.e. the depth of the central section of the acetabular canal in young people is 10-12 mm, and on average - 11.1 ± 0.5 mm. With age, the depth decreases. Thus, in the elderly it is 5-12 mm, on average 7.5 ± 0.37 mm, and in old age - 3.5 ± 0.25 mm (1972ПодрушнякЕП). According to our measurements on radiographs, on average, the depth of the acetabulum fossa in middle-aged and young people in women is 7.89 mm, in men - 8.99 mm, and for both sexes - 8.38 mm (2004Архипов-БалтийскийСВ). According to К.П. Минеев, К.К. Стэльмах (1996), the height of the slit-like space, i.e. the depth of the acetabular canal, is 4-8 mm. Accordingly, in mild osteoarthrosis and without protrusion, an arthroscope with a diameter of 4 mm will fit freely in the peripheral and central sections of the acetabular canal (Fig. 24).
 |
| Fig. 24. Dissection of the hip joint with a superimposed arthroscope inserted into the acetabular canal (from 1836WeberW_WeberE, with our additions). |
The arthroscope needs to penetrate the suprasynovial subsection of the acetabular canal, where the synovial fluid circulates. To do this, it is necessary to perforate the synovial membrane in the anteroinferior part of the bottom of the acetabular fossa (Fig. 25). Earlier, the guide wire will pass through the adipose tissue, either between the pubic and ischial portions of the LCF and exit in the mid-anterior part of the acetabular fossa, or emerge closer to the transverse ligament between the LCF and the anterior wall of the acetabular notch. Before introducing fluid or gas, it is essential to confirm, using all available methods, that the drainage system truly communicates with the joint cavity (wire, optical system, aspiration, trial saline injection, radiographic confirmation, etc.).
After the introduction of fluid or gas, it becomes possible to further expand the central compartment by gently applying manual traction to the operated leg. In the suprasynovial subregion, we will observe: the hyaline cartilage of the femoral head, the LCF, synovial folds, adipose tissue covered with synovial membrane, the walls of the acetabular fossa, and the inner edge of the articular cartilage of the lunate surface. The operator will visually assess the condition of these elements, test them with a hook probe, and evaluate them through movements of the femur.
 |
| Fig. 25. The central section of the acetabular canal and the contents of the central compartment. Left: the suprasynovial part with the LCF retracted and raised upward to show the falciform fold connecting it to the floor (the transverse ligament of the acetabulum is in place, we have drawn the arthroscope); 1 — LCF, 1’ — its pubic bundle; 1’’ — its sciatic bundle; 2 — bottom of the acetabulum; 3 — synovial fold running from the inner surface of the LCF to the pubic margin of the floor of the acetabular fossa; 4 — synovial space. On the right: subsynovial part with LCF raised upwards (transverse ligament of the acetabulum is removed); 1 — acetabulum, 1’ — its bottom, 1’’ — acetabular labrum; 2 — LCF; 3 — pubic bundle; 4 — its sciatic bundle; 5 — acetabular artery with 5’ — branch of LCF; 6 and 6’ — veins coming from the bottom of the acetabulum (from 1904TestutL, with our additions). |
Theoretically, it is possible to visualize the LCF subsynovially before penetrating into the free joint space. It seems to us that by careful pneumatic or hydropreparation and partial removal of fatty tissue, the proximal section of the LCF (pubic and ischial portions) and its vessels will become available for inspection (Fig. 25). The topography of the acetabular canal allows, in principle, to reinsert the proximal end, and in case of subsynovial ruptures, to suture, reconstruct and replace the LCF subsynovially. Even 19th century anatomists noted that the LCF is located extra-articularly, implying the presence of an "articular" and "extra-articular" part in the hip joint, delimited by the synovial membrane (1857RichetA). C.T. Aeby (1868) wrote: the synovial "tube" in which the LCF is located has an outlet to the outside through the acetabulum notch. The very structure of the human being invites us to use this route. This will eliminate the “contamination” of the intra-articular environment during surgery with blood cells, tissue detritus, bacteria, carbonized particles, and in the postoperative period, for example, with wear products of the LCF endoprosthesis and macrophages that have absorbed foreign microparticles.
 |
| Fig. 26. Human pelvis, left side view; we have added various positions of the arthroscope (exhibit of the Zoological Museum of Moscow State University, Moscow, photograph by the author). |
Having successfully penetrated the hip joint, we gain the ability to more confidently move the optical system in the sagittal plane (Fig. 26), and after manual distraction, in the frontal plane. At the diagnostic stage of arthroscopy, we believe that the risk of damaging large extra-articular vessels and nerves is minimal. Specialized endoscope shells and instruments, and a decrease in the diameter of the optics will allow surgical procedures to be performed in the central compartment through the lower portal. Its use does not exclude a combination with known lateral approaches. From the lower portal, it is also possible to examine the anteroinferior and posteroinferior parts of the peripheral compartment.
Our dream is to implement early diagnostics of hip pathology and LCF injuries using puncture microfibroscopy through the lower approach. Reducing invasiveness and eliminating distraction suggests the feasibility of the procedure under local or regional anesthesia.
[3]. Main Advantages of the Proposed
Technique
- Reducing the risk of complications associated with traction.
- Reducing the risk of complications associated with accessing the central compartment from the lateral side.
- Reduced cost of consumables for the operation.
- Cosmeticity of the operation.
- Less labor intensity and duration.
[4]. Specific Risks of the Proposed
Technique
- Damage to the vessels and nerves of the obturator fascicle.
- Penetration into the small pelvis through the obturator membrane.
- Penetration into the retroperitoneal space through the obturator canal.
- Puncture damage to the cartilaginous cover of the femoral head, transverse ligament, acetabular labrum and LCF.
[5]. Main Limitations of the Proposed
Technique
- Impossibility of introducing a second standard-sized instrument into the central compartment.
- Limited view of the peripheral compartment from the lower approach.
[6]. References
Aeby CT. Der Bau des menschlichen Körpers mit besonderer Rücksicht auf seine morphologische und physiologische Bedeutung Erste lieferung. Leipzig: F.C.W. Vogel, 1868.
Aprato A, Giachino M, Masse A. Arthroscopic approach and anatomy of the hip. Muscles, Ligaments and Tendons Journal. 2016;6(3)309-16. pmc.ncbi.nlm.nih.gov
Ayeni OR, Bedi A, Lorich DG, Kelly BT. Femoral neck fracture after arthroscopic management of femoroacetabular impingement: a case report. JBJS. 2019;3(9)e47. journals.lww.com
Badylak JS, Keene JS. Do iatrogenic punctures of the labrum affect the clinical results of hip arthroscopy? Arthroscopy. 2011;27:761-7. arthroscopyjournal.org
Bailey TL, Stephens AR, Adeyemi TF, Xu Y, Presson AP, Aoki SK, Maak TG. Traction time, force and postoperative nerve block significantly influence the development and duration of neuropathy following hip arthroscopy. Arthroscopy. 2019;35(10)2825-31. pubmed.ncbi.nlm.nih.gov
Bharam S. Labral tears, extra-articular injuries, and hip arthroscopy in the athlete. Clinics in sports medicine. 2006;25(2)279-92. academia.edu
Chan K, Farrokhyar F, Burrow S, Kowalczuk M, Bhandari M, Ayeni OR. Complications following hip arthroscopy: a retrospective review of the McMaster experience (2009–2012). Canadian Journal of Surgery. 2013;56(6)422-6. pmc.ncbi.nlm.nih.gov
Chiang CC, Tang HC, Yang CP, Sheu H, Chuang CA, Chan YS. Risk factors for insufficient hip distraction for safe central compartment access during hip arthroscopy: retrospective analysis of 677 cases. Journal of Hip Preservation Surgery. 20 February 2025; hnaf009.
Chapchal G. Orthopädische chirurgie und traumatologie der Hüfte. Stuttgart: Ferdinand Enke verlag, 1965.
Chen HH, Li AF, Li KC, Wu JJ, Chen TS, Lee MC. Adaptations of ligamentum teres in ischemic necrosis of human femoral head. Clin Orthop Relat Res. 1996;328:268-75. journals.lww.com
Cooper DE, Fouts B. Single-portal arthroscopy: Report of a new technique. Arthroscopy techniques. 2013;2(3)e265-9. sciencedirect.com
Debierre C. Traité élémentaire d'anatomie de l'homme (anatomie descriptive et dissection): avec notions d'organogénie et d'embryologie générale. Tome 1. Paris: Félix Alcan, 1890.
Degen RM, Bernard JA, Pan TJ, Ranawat AS, Nawabi DH, Kelly BT, Lyman S. Hip arthroscopy utilization and associated complications: a population-based analysis. Journal of hip preservation surgery. 2017;4(3)240-9. academic.oup.com
Dippmann C, Thorborg K, Kraemer O, Winge S, Hölmich P. Symptoms of nerve dysfunction after hip arthroscopy: an under-reported complication?. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014;30(2)202-7. sciencedirect.com
Duplantier NL, McCulloch PC, Nho SJ, Mather III RC, Lewis BD, Harris JD. Hip dislocation or subluxation after hip arthroscopy: a systematic review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016;32(7)1428-34. arthroscopyjournal.org
Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1999;15(2)132-7. citeseerx.ist.psu.edu
Frandsen L, Lund B, Grønbech Nielsen T, Lind M. Traction-related problems after hip arthroscopy. Journal of hip preservation surgery. 2017;4(1)54-9. pmc.ncbi.nlm.nih.gov
Frazer JES. Anatomy of the Human Skeleton. 2nd ed., London: J. & A. Churchill, 1920.
Gao F, Yang Y, Ma H. Tensile properties of iliac ligament versus femoral head ligament. J Clin Rehab Tissue Eng Res. 2008;26:5105-8. caod.oriprobe.com
Garbe S. Zwischen Biomechanik und Pathomechanik des Femurs. Bern [etc.]: Verlag Hans Huber, 1998.
Gray H. Anatomy, descriptive and surgical; 17th ed. Philadelphia, New York: Lea & Febiger, 1908.
Gupta A, Redmond JM, Hammarstedt JE, Schwindel L, Domb BG. Safety measures in hip arthroscopy and their efficacy in minimizing complications: a systematic review of the evidence. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014;30(10)1342-8. arthroscopyjournal.org
Gursoy S, Cirdi YU, Kirac M., Chahla J. Basics of hip arthroscopy: Step‐by‐step technique. Journal of Experimental Orthopaedics. 2024;11(2)e12021. esskajournals.onlinelibrary.wiley.com
Güven Ş, Veizi E, Naldöven ÖF, Erdoğan Y, Şahin A,
Mert HÇ, Fırat A. Traction-Related Urinary Complications in Hip Arthroscopy
using a perineal post: Prevalence, Risk Factors, and Outcomes. Orthopaedics
& Traumatology: Surgery & Research. 13 February 2025; 104187. sciencedirect.com
Humphry GM. A Treatise on the Human Skeleton including the Joints. Cambridge: MacMillan and Company, 1858.
Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: indications, outcomes and complications. International Journal of Surgery. 2018;54(B)341-4. sciencedirect.com
Kowalczuk M, Bhandari M, Farrokhyar F, Wong I, Chahal M, Neely S, Ayeni OR. Complications following hip arthroscopy: a systematic review and meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21:1669-75. academia.edu
Lo YP, Chan YS, Lien LC, Lee MS, Hsu KY, Shih CH. Complications of hip arthroscopy: analysis of seventy three cases. Chang Gung Med J. 2006;29(1)86-92. cgmj.cgu.edu.tw
Loder JC. Tabulae anatomicae quas ad illustrandam humani corporis fabricam collegit et curavit. Vinariae, 1794.
Maldonado DR, Chen JW, Walker-Santiago R, Rosinsky PJ, ShapiraJ, Lall AC, Domb BG. Forget the greater trochanter! Hip joint access with the 12 o’clock portal in hip arthroscopy. Arthroscopy Techniques. 2019;8(6)e575-84. sciencedirect.com
Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2009;25(4)400-4. arthroscopyjournal.org
McCarthy JC, Day B, Busconi B. Hip arthroscopy: applications and technique. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 1995;3(3)115-22. andreassauerbreymd.com
Nakano N, Khanduja V. Complications in hip arthroscopy. Muscles, Ligaments and Tendons Journal. 2016;6(3)402-9. pmc.ncbi.nlm.nih.gov
Netter F. Atlas of human anatomy. 6th ed. Philadelphia: Saunders Elsevier, 2011.
Palletta GB. Exercitationes pathologicae. Mediolani: Societas Typ. e Classicis Scriptoribus Italicis, MDCCCXX [1820].
Papavasiliou AV, Bardakos NV. Complications of
arthroscopic surgery of the hip. Bone Joint Res 2012;1(7)131-44. boneandjoint.org.uk
Parvizi J, Bican O, Bender B, Mortazavi SJ, Purtill JJ, Erickson J, Peters C. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. The Journal of arthroplasty. 2009;24(6)110-3. academia.edu
Philippon MJ, Rasmussen MT, Turnbull TL, Trindade CA, Hamming MG, Ellman MB, Harris M, LaPrade RF, Wijdicks CA. Structural Properties of the Native Ligamentum Teres. Orthop J Sports Med. 2014;2(12)2325967114561962. journals.sagepub.com
Poirier P.J. Traité d'anatomie humaine. Tome 1, Fascicule 2 / par MM. A. Charpy, ... A. Nicolas, ... A. Prenant, ... E. Jonnesco; publié sous la direction de Paul Poirier. Paris: L. Battaille et Cie, 1892.
Richet A. Traité pratique d' Anatomie medico-chirurgicale. Paris: F. Chamerot, 1857.
Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2008;24(9)1019-26. sciencedirect.com
Rüdinger N. Die Gelenknerven des menschlichen Körpers. Erlangen: F. Enke, 1857.
Said HG, Steimer O, Kohn D, Dienst M. Vascular obstruction at the level of the ankle joint as a complication of hip arthroscopy. Arthroscopy. 2011;27(11)1594-6. arthroscopyjournal.org
Salas AP Mazek J, Araujo-Reyes D, Gonzalez-Campos M, Castillo-Trevizo A, Garcia JM. The Tutankhamun technique in hip arthroscopy. Arthroscopy techniques. 2018;7(11)e1167-71. sciencedirect.com
Salas AP, Mazek J, María AC, Taffinder DS, Velasco-Vazquez H. Hip Arthroscopy in Adolescents Through an Extra-Capsular Approach. Arthroscopy Techniques. 2023;12(6)e867-71. arthroscopytechniques.org
Salas AP. Radiographic and anatomic landmarks to approach the anterior capsule in hip arthroscopy. Journal of Hip Preservation Surgery. 2015;2(4)431-7. academic.oup.com
Schwencke T. Haematologia, sive sanguinis historia, experimentis passim superstructa. Accedit observatio anatomica de acetabuli ligamento interno, caput femoris firmante, cum binis tabulis adjectis. Hagae: Jon. Mart. Husson, 1743.
Seijas R, Ares O, Sallent A, Cuscó X, Álvarez-Díaz P, Tejedor R, Cugat R. Hip arthroscopy complications regarding surgery and early postoperative care: retrospective study and review of literature. Musculoskeletal surgery. 2017;101:119-31. academia.edu
Simpson J, Sadri H, Villar R. Hip arthroscopy technique and complications. Revue de chirurgie orthopédique et traumatologique. 2010;96(8)S287-95. sciencedirect.com
Steinberg ME. Avascular necrosis of the femoral head. In: Surgery of the hip joint; еd. R.G. Tronzo. 2nd ed. Berlin [etc.]: Springer-Verlag, 1984;2:1-29.
Stone AV, Howse EA, Mannava S, Miller BA, Botros D, Stubbs AJ. Basic hip arthroscopy: Diagnostic hip arthroscopy. Arthroscopy Techniques. 2017;6(3)e699-704. arthroscopytechniques.org
Tang HC, Brockwell J, Dienst M. Hip arthroscopy via a peripheral compartment first capsular-preserving technique: a step-by-step description. Journal of Hip Preservation Surgery. 2020;7(3)596-603. academic.oup.com
Telleria JJ, Safran MR, Gardi JN, Harris AH, Glick JM. Risk of Sciatic Nerve Traction Injury During Hip Arthroscopy—Is It the Amount or Duration?: An Intraoperative Nerve Monitoring Study. JBJS. 2012;94(22)2025-32. journals.lww.com
Testut L. Traité d'anatomie humaine. Tome 1. Osteologie – Arthrologie – Miologie. Cinquième édition, revue, corrigée et augmentee. Paris: Octave Doin, 1904.
Weber W, Weber E. Mechanik der menschlichen Gehwerkzeuge: eine anatomisch-physiologische Untersuchung. Gottingen: Dietrichsche Buchhandlung, 1836.
Архипов-Балтийский С.В. Рассуждение о морфомеханике. Норма: В 2-х томах. Калининград, 2004.
Воробьев ВН. Элементы капсулы тазобедренного сустава и оперативные доступы к нему. Ортопед., травматол. 1972;1:21-6.
Воробьев ВП. Анатомия человека: Руководство и атлас для студентов и врачей. В 3 томах, Т.1. Москва: Медгиз, 1932.
Геселевич АМ, Лубоцкий ДН. Пособие к практическим занятиям по топографической анатомии конечностей. Куйбышев, 1941.
Голуб ДМ, Бронивицкая ГМ. Развитие тазобедренного сустава и его иннервации у человека. Архив анатом., гистол. и эмбриол. 1981;80(5)47-5.
Грум К. Монографиiя о радикальномъ леченiи пахомошоночныхъ грыжъ, въ особенности по способу, основанному на двадцати семи операцiяхъ; съ подробнымъ анатомическимъ, физiологическимъ и патологическим разсужденiемъ о паховыхъ грыжахъ вообще, и практическимъ разборомъ главнѣйшихъ методъ ихъ радикальнаго леченiя. С присовокупленiемъ записки его о отнятiи членовъ, и изъятiи изъ суставовъ, операцiй, производимыхъ на полѣ сраженiя. САНКТПЕТЕРБУРГЪ: въ типографiи Министерства внутреннихъ дѣлъ, 1837.
Кованов ВВ, Травин АА. Хирургическая анатомия нижних конечностей. Москва, 1963.
Малахова СО. Артроскопия тазобедренного сустава (клинико-экспериментальное исследование): дис. … канд. мед. наук. Москва, 2001.
Минеев К. П. Операции на покровах тела и конечностях: учеб. пособие. Ульяновск: Симбирская книга, 1995.
Минеев К.П., Стэльмах К.К. Лечение тяжелых повреждений таза и позвоночника. Ульяновск: Симбирская книга, 1996.
Николаев ЛП. Руководство по биомеханике в применении к ортопедии, травматологии и протезированию. Киев: Гос. мед. издат. УССР, 1947.
Обысов АС. Надежность биологических тканей. Москва: Медицина, 1971.
Перлин БЗ, Андриеш ВН, Бибикова ЛА. Иннервация тазобедренного сустава человека в норме и при туберкулезном коксите. Кишинев: Штиинца, 1977.
Подрушняк ЕП. Возрастные изменения суставов человека. Киев: Здоров‘я, 1972.
Синельников РД, Синельников ЯР. Атлас анатомии человека: учеб. пособие; 2-е изд. в 4-х т. Москва: Медицина, 1996.
Address correspondence to Arkhipov Sergey, M.D., E-mail: archipovsv@gmail.com
Cite
Keywords
ligamentum capitis
femoris, ligamentum teres, ligament of head of femur, acetabular canal, inferior
portal, arthroscopy
Additions
The article was supplemented with a quote on 20.01.2025.
Design update, correction, and addition of the article, February 8,
2025.
The article was supplemented on 02.03.2025.
History of the article:
First publications in the online magazine:
Arkhipov SV. Inferior Portal for Hip Arthroscopy: A Pilot Experimental Study. Pt. 1. Background and Hypothesis. About Round Ligament of Femur. January 18, 2025. https://roundligament.blogspot.com/2025/01/lower-portal.html
Arkhipov SV. Inferior Portal for Hip Arthroscopy: A Pilot Experimental Study. Pt. 2. Inferior Portal Prototypes. About Round Ligament of Femur. February 8, 2025. https://roundligament.blogspot.com/2025/02/inferior-portal-part-2.html
Combined PDF version:
Arkhipov SV. Inferior Portal for Hip Arthroscopy: A Pilot Study. About Round Ligament of Femur. February 26, 2025. https://roundligament.blogspot.com/2025/02/inferior-portal-for-hip-arthroscopy.html; DOI: 10.13140/RG.2.2.27152.93449, www.researchgate.net, academia.edu, Google Drive
NB! Fair practice / use: copied for the purposes of criticism, review, comment, research and private study in accordance with Copyright Laws of the US: 17 U.S.C. §107; Copyright Law of the EU: Dir. 2001/29/EC, art.5/3a,d; Copyright Law of the RU: ГК РФ ст.1274/1.1-2,7











Comments
Post a Comment