Invention (Patent Application Publication): Howald R,
Heuberger P, Trommsdorff U. Implant, WO2007090790A2 (2007).
WO2007090790A2 Switzerland
Inventors: Ralph Howald, Peter Heuberger, Ulrike Trommsdorff
Worldwide applications 2007 WO EP US
Application PCT/EP2007/051008 events:
2007-02-02 Application filed by Zimmer Gmbh
2007-02-02 Priority to US12/278,835
2007-02-02 Priority to EP07726285A
2007-08-16 Publication of WO2007090790A2
2007-12-06 Publication of WO2007090790A3
Implant
Ralph
Howald, Peter Heuberger, Ulrike Trommsdorff
Abstract
The invention relates to an implant for the relief of
damaged regions of the joint surfaces of hip or shoulder joints which may be
introduced into the gap between the joint surfaces of the joint head (11) and
the joint socket (13) in the natural joint, the implant being embodied as a
shell or cap which is laid in the implanted state with a convex outer surface
(29) in the joint socket (13) and a convex inner surface (31) sitting on the
joint head (11). The implant has a body section (15, 17) forming the shell or
cap with an opening (27) and a boundary section (19) defining the opening (27)
and the implant is made from a flexible material which may be deformed for
introduction of the implant into the gap between the joint surfaces.
Description
The invention relates to an implant for the relief of
damaged areas of the articular surfaces of hip or shoulder joints.
In known joint
prostheses usually both articular surfaces are replaced by coordinated
artificial joint parts. As is known, this takes place within the scope of
surgery, in which a more or less large part of the healthy bone is removed,
depending on the prosthesis used in each case. In hip surgery, for example, the
femoral head is partially or completely removed to make room for a condyle that
is usually anchored in the femur via a shaft. Accordingly, at the acetabulum
(acetabulum) of the hip bone by appropriate processing during surgery bone
material removed to attach an artificial socket or joint cup can, which serves
to accommodate the artificial condyle.
Such operations are
associated with considerable burdens and risks for the patient. A problem
particularly in relatively young patients is that proper function of an
artificial joint can not be guaranteed for any length of time. In many cases,
follow-up surgery is required. However, such revisions are often difficult to
carry out, since even the first operation has cost the patient a not
inconsiderable part of the healthy bone material.
The first surgery
that results in relevant loss of bone material may be delayed by so-called
resurfacing techniques become. Here, only the surfaces of the affected joints
are replaced by comparatively thin, cap or cup-shaped implants. However, these
known techniques require stressful operations, which are also not minimally invasive
possible. Furthermore, resurfacing also requires the removal of healthy bone
material in the area of the involved articular surfaces, albeit to a lesser
extent than in the aforementioned operations.
These considerations
are especially important when the articular surfaces are affected by arthrosis
and the involved bones themselves are intact, i. E. no fractures need to be
treated. Such joint damage also occurs in relatively young patients, which is
why there is a need for techniques for the treatment of damaged joint surfaces,
in which the healthy bone material should remain as possible. To minimize the
burden on the patient, such techniques should be minimally invasive.
It is the object of
the invention to provide an implant which meets these requirements.
The invention
provides an implant for relief of damaged areas of the articular surfaces,
which can be introduced into the gap between the interacting in the natural
joint articular surfaces of the condyle and the acetabulum, wherein the implant
is designed as a shell or cap in the implanted state with a convex Outer side
is located in the socket and sits with a concave inner side on the condyle,
wherein the implant comprises a shell or cap forming body portion having an
opening, and an edge portion which defines the opening, and wherein the Implant
is made of a flexible material which is deformable for introducing the implant
in the existing between the joint surfaces gap.
The implant can
significantly reduce pressure and / or shear loads on arthrosis affected areas
of the articular surfaces. As a result, the implant is not exclusively
suitable, but especially well for joints affected by osteoarthritis in the
early stages.
The time at which a
first operation of the type described above becomes inevitable, can be pushed
out through the implant. Therefore, the implant is not exclusive, but
especially interesting for relatively young patients.
The advantage is
that the implant can be used as part of a minimally invasive procedure. There
is no processing of the bone required. The implant can be designed so that it
aligns itself in the joint space. Alternatively, the implant can be fixed to
the natural bone or tissue structures.
Furthermore, it is
advantageous that the insertion of the implant does not require subluxation of
the condyle.
It has been found
that by a suitable material and / or by a suitable material coating for the
implant, the natural joint function can be maintained upright.
The implant can be
made of one or more different metallic or non-metallic materials. In question
is, for example, a hydrogel, polyurethane or polyethylene. The implant may
contain a textile material or consist of a textile material, wherein the
textile material comprises a textile substrate, and wherein at least on a part of
the surface of the textile substrate, a coating is provided which is one of the
hydrogels, polyurethanes, polyvinyl chloride, Polytetrafluoroethylene and any
combination of two or more of the aforementioned compounds selected compound.
The textile substrate
may be made of fibers, at least a portion of the fibers being provided with a
coating containing a compound selected from the group consisting of hydrogels,
polyurethanes, polyvinylchloride, polytetrafluoroethylene and any combination
of two or more of the aforementioned compounds.
This makes it
possible to realize gliding properties that at least largely correspond to the
natural conditions in the joint.
Furthermore, the
implant may have a sandwich construction of a plurality of individual layers.
At least two layers may differ from one another in terms of their construction
and / or their material.
The implant or at
least one layer of a sandwich construction of the implant comprising a
plurality of individual layers may be provided with a textile, fibrous, braid,
knit or fabric reinforcement.
Two adjacent layers,
which have the same material but a different structure, can be chemically mixed
with one another be, wherein the crosslinking was generated for example by
irradiation.
The material of the
implant may be bioresorbable.
Furthermore, it can
be provided that the implant comprises a plurality of respectively a partial
area of the outside and / or the inside forming relief elements. The relief
elements can be designed as upholstery, cushions or bales. The relief elements
can be connected to each other by a flat support structure. The support
structure may comprise a textile, fiber, braid, knit or fabric material.
The edge portion may
be provided with a reinforcement. In the edge section separate strength carrier
can be integrated. A reinforcement of the edge portion can be made by a fiber
or cord structure.
It is also possible
that the edge portion is hollow and provided with a filling. The filling may be
a gas, for example air, or a liquid. It may be provided a filler whose state
changes with time. While the filler material is liquid or pasty upon insertion
of the implant to facilitate insertion, over time, the filler material
transitions to a solid state such that the rim portion imparts high dimensional
stability to the implant and / or for stable positioning of the implant between
the two articular surfaces.
The body portion of
the implant may comprise a ball portion and a cylinder portion, the cylinder
portion being attached to the ball portion. cut connects. The ball portion may
have the shape of a hemisphere.
The edge portion may
be thickened relative to the wall thickness of the body portion. It can be
provided that the edge portion is formed bead-shaped.
Depending on the
respective joint, the implant can be dimensioned such that in the implanted
state the edge section is located outside the gap existing between the joint
surfaces.
In order to
facilitate deformation of the implant during insertion and / or to take into
account the anatomy of the relevant joint, the body portion of the implant may
have at least one recess. When used on the hip, this recess can serve to
preserve the so-called Hüftkopfband (ligamentum capitis femoris).
The recess may
extend into the edge portion, wherein the edge portion may have an interruption
formed by the recess. A separate fitting may be provided which, after inserting
the implant into the gap between the articular surfaces, may be inserted into
the interruption of the rim portion to close the rim portion. The fitting can
thus give the implant in the inserted state dimensional stability again.
It is possible, but
not mandatory, for the implant to have a constant wall thickness. If a recess
of the type described above is provided, then the wall thickness of the body
portion of the vary in that the wall thickness near the recess is greater than
in the region further away from the recess.
In one possible
embodiment, a wall thickness distribution results in that, starting from a
symmetrical state in which the body portion has a constant wall thickness
between the inside and the outside, the inside and the outside are shifted from
one another. This offset may be in a direction parallel to an equatorial plane
of a sphere portion of the body portion.
If a recess of the
type described above is provided, then the offset of the inside relative to the
outside in a direction away from the recess. This results in a distribution of
the type already mentioned above, according to which the wall thickness in the
area of the recess is greater than in areas removed from the recess.
Other possible
embodiments will be apparent from the dependent claims, the description and the
drawings.
The invention will
now be described by way of example with reference to the drawings. Show it:
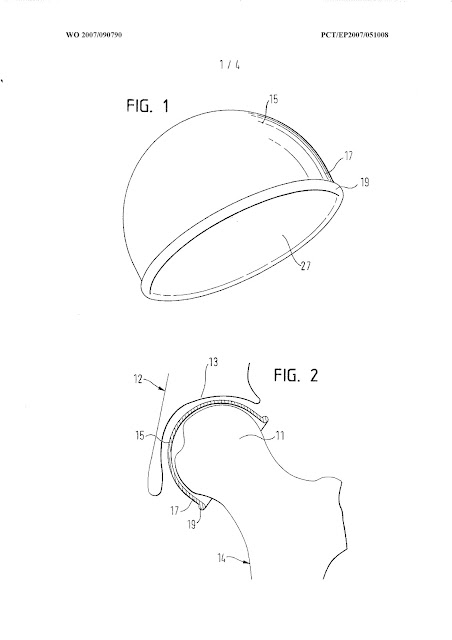
Fig. 1-3 an embodiment of an implant according to the invention,
and
Fig. 4-7, another
embodiment of an implant according to the invention. The implant can be used
for both hip joints and shoulder joints. Two embodiments will be explained
below, for example only in connection with the hip joint.
The implant
according to FIGS. 1 to 3 is designed as a cap, which comprises a sphere
section 15 in the form of a hemisphere. At the ball portion 15, a cylindrical
portion 17 connects.
The cap is open at
the bottom. The opening 27 is delimited by an edge section 19. The edge portion
19 comprises a bead-shaped thickening such that the edge portion 19 projects
radially outward relative to the cylinder portion 17.
The insertion of the implant can take place within the
framework of an arthroscopic procedure. The joint Surfaces can be separated,
for example, e.g. by use of an extraction table, and indeed without subluxation
of the femoral head 11. The insertion of the implant can also take place by
other minimally invasive procedures.
The implant consists of a flexible material. In this way, the implant can be deformed
during insertion and adapt to the shape of the joint gap between the femoral
head 11 and the socket 13. With regard to the possible materials or the
possible structure of the implant, reference is also made to the introductory
part.
The material may be
metallic or non-metallic. In question is, for example, a hydrogel, polyurethane
or polyethylene. The material can be reinforced by fiber or canvas structures.
Furthermore, the material can consist of several layers or layers, which are
either made of different materials or of the same material with the same
material. Different structures are made. The implant material may comprise a
substrate and a substrate coating. The substrate may be a textile material.
For example,
referring to FIG. 3, the inner radius A of the ball portion and the cylinder
portion may be in the range of 38-60 mm. The length D of the cylinder portion
17 is, for example, half of the inner radius A or less. The cylinder portion 17
may be arbitrarily short, with a cylinder portion 17 can be completely
dispensed with.
The wall thickness C
of the implant is constant and is for example 0.5 to 3 mm.
The bead-shaped edge
portion 19 is at least approximately circular in cross section. The radius E of
the bead is, for example, in the range of 0.5 to 4.0 times the wall thickness
C.
The bead-shaped edge
portion 19 may be solid and made entirely of the same material as the body
portion formed by the ball portion 15 and the cylinder portion 17.
Alternatively, the edge portion 19 may be reinforced by a cord structure, for
example. It is also possible to make the edge section 19 hollow and to be
filled with a gas, a liquid or a material which over the course of time changes
from a liquid or pasty initial state to a solid final state, as explained in
the introductory part.
With a corresponding
configuration, the bead-shaped edge portion 19 can ensure that the implant aligns
itself in the inserted state. In order to prevent relative movements between
the implant and the socket pan 13 or to reduce the extent of these movements
when moving the joint, the implant can be fastened to the edge area of the
acetabulum, namely on the bone or on the fibrocartilaginous material of the
labrum acetabuli.
It is also possible
to fasten the edge section 19 of the implant to the femoral neck, wherein a
possibly provided cord reinforcement of the edge section 19 can be used. As a
result, femoral articulation of the implant can be prevented or reduced in its
extent.
The embodiment
according to FIGS. 4 to 7 differs from the exemplary embodiment according to
FIGS. 1 to 3 by a recess 21 provided in the body section 15, 17 and by a
non-constant wall thickness.
The recess 21 extends from the ball section 15 via the
cylinder section 17 into the edge section 19. The edge section 19 is interrupted due to the recess 21. In order to
close the interruption again after insertion of the implant and to restore the
dimensional stability of the implant, a separate fitting piece 23 is provided.
When inserting the
implant, the fitting piece 23 is removed. The implant is pushed from the
cranial edge of the acetabulum 13 between the articular surfaces of the femoral
head 1 1 and the hip bone 12. Here, the flexible implant adapts itself to the
shape of the joint surfaces. As already mentioned, due to the recess 21 the
ligamentum capitis femoris 33, which is located in the implanted state in the
region of the recess 21 (FIG. 5).
The edge portion 19
can then be closed by the fitting piece 23. As a result, the implant again
acquires a dimensional stability in accordance with the exemplary embodiment
without a recess according to FIGS. 1 to 3.
A slight asymmetry
in wall thickness distribution, as described below, provides the implant with
rotational stability. Stability to rotation can also be achieved by fixing the
edge section 19 of the implant at the edge region of the acetabulum 13.
With regard to the
material and the structure of the implant, reference is made to the
explanations of the embodiment of FIG. 1 to 3.
The non-uniform wall
thickness distribution of the implant arises as a result (FIG. 6) that the
outer side 29 and the inner side 31 are displaced from one another with a
constant wall thickness starting from a symmetrical state along a line k, which
runs parallel to an equatorial plane Q. In other words, the outer side 29 and
the inner side 31 form two eccentrically adjacent spherical partial surfaces.
The direction of the displacement is chosen such that the inner side 31 is
displaced away from the recess 21. The center Ma of the inner side 31 thus lies
on the side of the center Mb of the outer side 29 facing away from the recess
21.
In this case, these center points Ma, Mb and the
center O of a circular region of a projection of the recess 21 lie on the
equatorial plane Q on a line k (FIG. 7). The circular area with Telpunkt O has a diameter G, which is basically
arbitrary, as long as the recess 21 does not reach to the pole of the implant
(Fig. 6). It is therefore possible to define two half-spaces which are
separated from each other by a plane T in which the center Mb of the outer side
29 lies, through which the center axis Zb of the corresponding outer surface of
the cylinder section 17 extends. In the one half space is the recess 21, while
in the other half space of the center Ma of the inner side 31 and the central
axis Za of the corresponding inner surface of the cylinder portion 17 are.
The size of the inner
radius A and the length D of the cylinder portion 17 may be sized according to
the embodiment of FIG. 1 to 3. The difference between outer radius B and inner
radius A is, for example, in the range of 0.5 to 3 mm. The radius E of the
bead-shaped edge portion 19 is, for example, in the range of 0.5 to 3.0 times
the aforementioned difference between outer radius B and inner radius A.
The offset F between
the two centers Ma and Mb and thus the central axes Za, Zb can be up to 2.5 mm.
The above-explained
direction of the offset F along the line k results in the greater wall
thickness in the region of the recess 21 and thus in the caudal region of the
acetabulum.
As an alternative to
the materials and the structure of the implant, as explained above and in connection
with the exemplary embodiment according to FIGS. 1 to 3, the implant can
consist of a plurality of soft individual elements which are formed in a
cushion, pillow or bale shape and serve as relief elements. The relief Elements
define the contact surfaces of the implant to the articular surfaces of the
femoral head 1 1 and the acetabulum 13 and thus serve to relieve already
damaged areas of the articular surfaces. The relief elements are interconnected
by a flat support structure, which may consist of a metallic or non-metallic
material. The support structure may comprise a textile, fiber, braid, knit or
fabric material.
In each of the
described embodiments, the invention provides an implant, by means of which the
damaged areas of the joint surfaces can be relieved. This relief can cause the
damaged areas to recover. Patient-burdening operations that result in the loss
of healthy bone can be delayed in this way. As already explained, this is of
great advantage, above all for relatively young patients.
LIST OF REFERENCES
11 condyle
12 hip bones
13 socket
14 femur
15 ball section 17
cylinder section
19 edge section
21 recess 23 fitting
piece
27 opening
29 outside
31 inside
33 Ligament of
capitis femoris
A inner radius
B outer radius
C Wall thickness of
the body section
D length of the
cylinder section
E radius of the
bead-shaped edge section
F offset
G diameter of the
circular area of the recess
O center of the
circular area of the recess
Q equatorial plane
T level
Ma center of the inside
Mb center of the
outside
Za central axis of
the inner surface of the cylinder portion
For example, center
axis of the outer surface of the cylinder portion k connecting line between Ma
and Mb
Claims:
1. An
implant for relieving damaged areas of the articular surfaces of hip or
shoulder joints, which can be introduced into the gap between the articular
joint surfaces of the joint head (11) and the joint socket (13), wherein the
implant is designed as a shell or cap, which is located in the implanted state
with a convex outer side (29) in the socket (13) and with a concave inner side
(31) on the condyle (11) sits, said implant forming a shell or cap body portion
(15, 17) and having an edge portion (19) defining the opening (27), and wherein
the implant is made of a flexible material that is deformable for insertion of
the implant into the gap present between the articular surfaces ,
2. Implant according to claim 1, characterized in that the
implant is made of one or more different non-metallic materials, for example of
a hydrogel, polyurethane or polyethylene.
3. Implant according to claim 1 or 2, characterized in that
the implant contains a textile material or consists of a textile material,
wherein the textile material comprises a textile substrate, and wherein at
least on a part of the surface of the textile substrate a coating is provided
which is one of hydrogels, polyurethanes, polyvinyl chloride,
polytetrafluoroethylene and any combination of two or more of the
aforementioned compounds.
4. Implant according to one of the preceding claims,
characterized in that the implant contains a textile material or consists of a
textile material, wherein the textile material comprises a textile substrate,
and wherein the textile substrate consists of fibers and at least a part of the
Fibers are provided with a coating which contains a compound selected from the
group consisting of hydrogels, polyurethane, polyvinyl chloride,
polytetrafluoroethylene and any combination of two or more of the
aforementioned compounds.
5. Implant according to one of the preceding claims,
characterized in that the implant is made of a bioresorbable material.
6. Implant according to one of the preceding claims,
characterized in that the implant has a sandwich construction of a plurality of
individual layers.
7. Implant according to claim 6, characterized in that at
least two layers differ from each other in terms of their structure and / or
their material.
8. Implant according to one of the preceding claims,
characterized in that the implant or at least one layer of a sandwich
construction of the implant, which has a plurality of individual layers, with a
textile, fiber, braid, knitted or Gewebever strengthening is provided.
9. Implant according to one of claims 6 to 8, characterized
in that two adjacent layers, which have the same material, but a different
structure, are chemically crosslinked with each other, wherein the crosslinking
was generated for example by irradiation.
10. Implant
according to one of the preceding claims, characterized in that the implant
comprises a plurality of each a portion of the outer side (29) and / or the
inner side (31) forming relief elements, which are each formed as a cushion,
cushion or bale, wherein the relief elements are interconnected by a flat
support structure.
1 1. Implant
according to claim 10, characterized in that the support structure is a
textile, fiber, mesh, or Gewirk Includes fabric material.
12. Implant according to one of the preceding claims,
characterized in that the edge portion (19) is provided with a reinforcement.
13. Implant according to one of the preceding claims,
characterized in that in the edge portion (19) separate strength members are
integrated.
14. Implant according to one of the preceding claims,
characterized in that the edge portion (19) is reinforced by a fiber or cord
structure.
15. Implant according to one of the preceding claims,
characterized in that the edge portion (19) is hollow and provided with a
filling.
16. Implant according to one of the preceding claims,
characterized in that the body portion comprises a ball portion (15) and a
cylinder derabschnitt (17), which adjoins the ball portion (15).
17. Implant according to claim 16, characterized in that the
ball portion (15) is a hemisphere.
18. Implant according to one of the preceding claims,
characterized in that the edge portion (19) is formed so that it gives the body
portion (15, 17) in the implanted state dimensional stability.
19. Implant
according to one of the preceding claims, characterized in that the implant is
dimensioned such that in the implanted state, the edge portion (19) is located
outside of the existing gap between the Gelenkflä-gap.
20. Implant according to one of the preceding claims,
characterized in that the edge portion (19) opposite the wall thickness C of
the body portion (15, 17) is thickened.
21. Implant according to one of the preceding claims,
characterized in that the edge portion (19) is formed bead-shaped.
22. Implant according to one of the preceding claims,
characterized in that the body portion (15, 17) has a recess (21).
23. Implant according to claim 22, characterized in that the
recess (21) extends into the edge portion (19) and the edge portion (19) has an
opening formed by the recess (21).
24. An implant according to claim 23, characterized in that
a separate fitting piece (23) is provided, which after the introduction of the
implant into the gap between the joint surfaces in the interruption of the edge
portion (19) is insertable to close the edge portion (19).
25. Implant according to one of claims 22 to 24,
characterized in that the wall thickness of the body portion (15, 17) near the
recess (21) is greater than in the recess (21) further away regions.
26. Implant according to one of the preceding claims,
characterized in that, starting from a symmetrical state in which the body
portion (15, 17) has a constant wall thickness between the inside (31) and the
outside (29), the inside (31) and the outer side (29) are shifted from each
other.
27. Implant according to claim 26, characterized in that the implant has a recess (21) and the inner side (31) is displaced in a direction away from the recess (21).
External links
Howald R, Heuberger P, Trommsdorff U. Implant. WO2007090790A2 February 2, 2006. 2007. patents.google [Deu]
Howald R, Heuberger P, Trommsdorff U. Implant and a method for partial replacement of joint surfaces. US20090048679A1 February 2, 2006. 2009. patents.google [Eng]
Publications
of invention
EP1965736 (A2)
US2009048679 (A1)
WO2007090790 (A2)
WO2007090790 (A3)
2007HowaldR_TrommsdorffU
Authors & Affiliations
Ralph Howald,
Gossau (CH)
Peter Heuberger,
Raterschen (CH)
Ulrike
Trommsdorff, Zurich (CH)
Keywords
ligamentum capitis femoris, ligamentum teres, ligament
of head of femur, endoprosthesis, prosthesis,
invention, unipolar, subtotal
NB! Fair practice / use: copied for the purposes of criticism, review, comment, research and private study in accordance with Copyright Laws of the US: 17 U.S.C. §107; Copyright Law of the EU: Dir. 2001/29/EC, art.5/3a,d; Copyright Law of the RU: ГК РФ ст.1274/1.1-2,7




Comments
Post a Comment